A Novel Use of Apremilast for the Treatment of Erythema Multiforme: A Case Report
CR2
Marianne Dobson
Marianne Dobson, Alyson Brown, Elizabeth Theaker
Title: A Novel Use of Apremilast for the Treatment of Erythema Multiforme: A Case Report
Authors: Marianne Dobson, Alyson Brown, Elizabeth Theaker
Background:
Erythema multiforme (EM) is an immune-mediated self-limiting mucocutaneous condition typically triggered by infections, most commonly Herpes Simplex Virus Type 1, and medications. Some triggers are unknown.
Management focuses on treating the underlying triggering condition and symptomatic relief. Management of severe recurrent or refractory cases can be challenging and may necessitate systemic immunosuppression. Choosing a suitable systemic agent can be challenging, particularly when a conventional immunosuppressive agent is contraindicated or unacceptable to the patient.
Apremilast is a phosphodiesterase type-4 inhibitor which suppresses synthesis of pro-inflammatory mediators (e.g. IL-12) and promotes anti-inflammatory mediators (e.g. IL-17A) It is licensed to treat severe psoriasis, psoriatic arthritis and Behçets disease. Its use in EM has not been widely explored with only 4 case reports published to date.
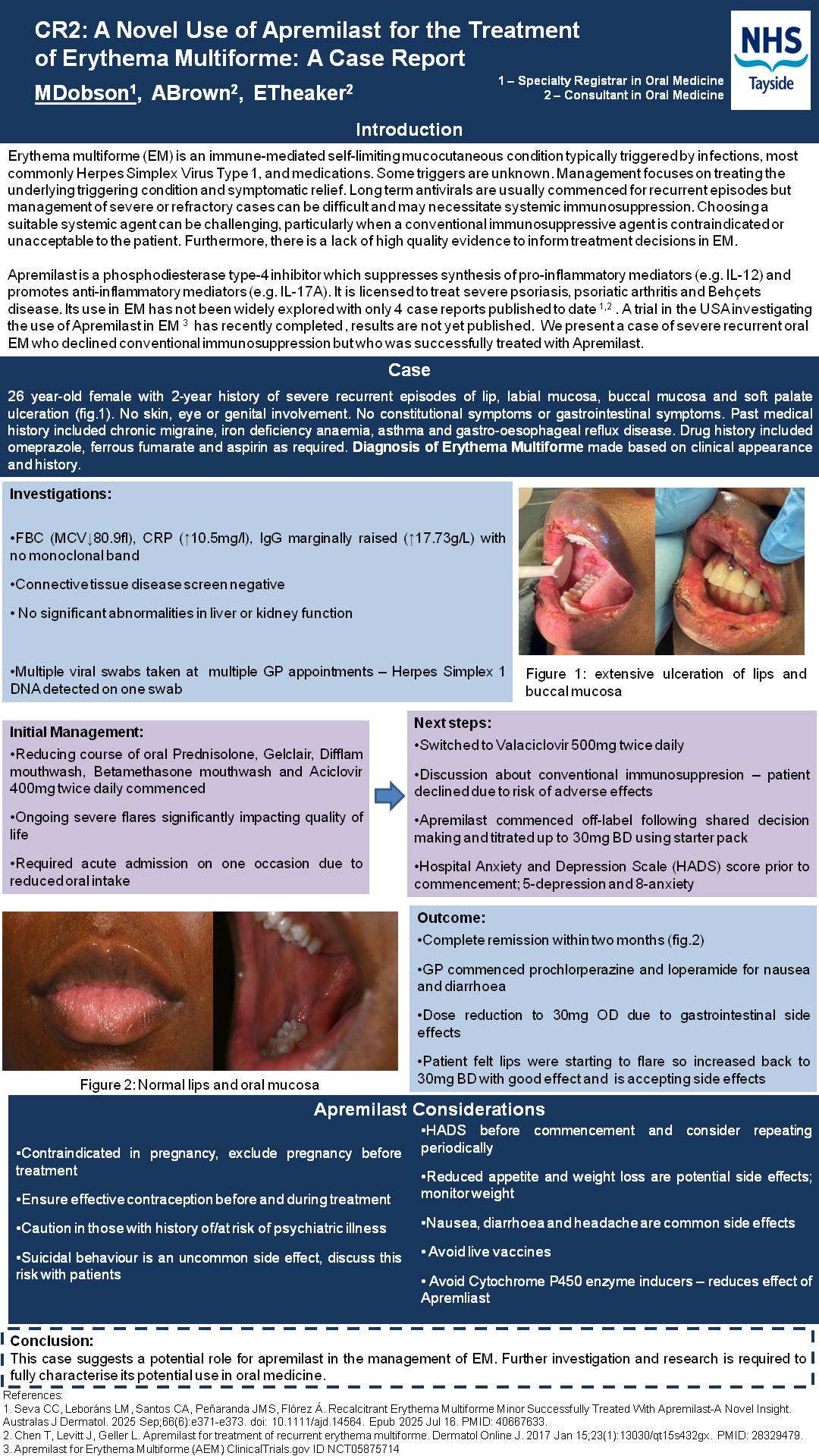
Case: We present the case of a 26 year-old female with a 2 year history of severe recurrent oral EM. Despite prophylactic antivirals and corticosteroids she experienced frequent monthly flares impacting her quality of life and requiring acute admission on one occasion. Haematological, immunological and biochemical blood investigations were largely unremarkable. The patient declined the option of a DMARD due to risk of adverse effects. Apremilast was commenced on an off label basis following shared decision making. The dose was titrated to 30mg twice daily with significant reduction in lesion frequency and severity with complete remission within two months. Gastrointestinal side effects necessitated a subsequent dose reduction.
Conclusion: We present a case of recurrent severe oral EM successfully treated with apremilast. This case suggests a potential role for apremilast in the management of EM. Further investigation and research is required to fully characterise it’s potential use in oral medicine. Clinicians should monitor for suicidal ideation and be aware that gastrointestinal side effects may limit dose.