Epidemiological Trends and Demographic Patterns of Head and Neck Cancer in Jordan: Preliminary Analysis from a National Cancer Registry (2000–2022)
OR2
Shaima Abujaber
Shaima Abujaber ¹, Prof. Gerry McKenna ¹, Dr Amanda Willis ²
Objectives:
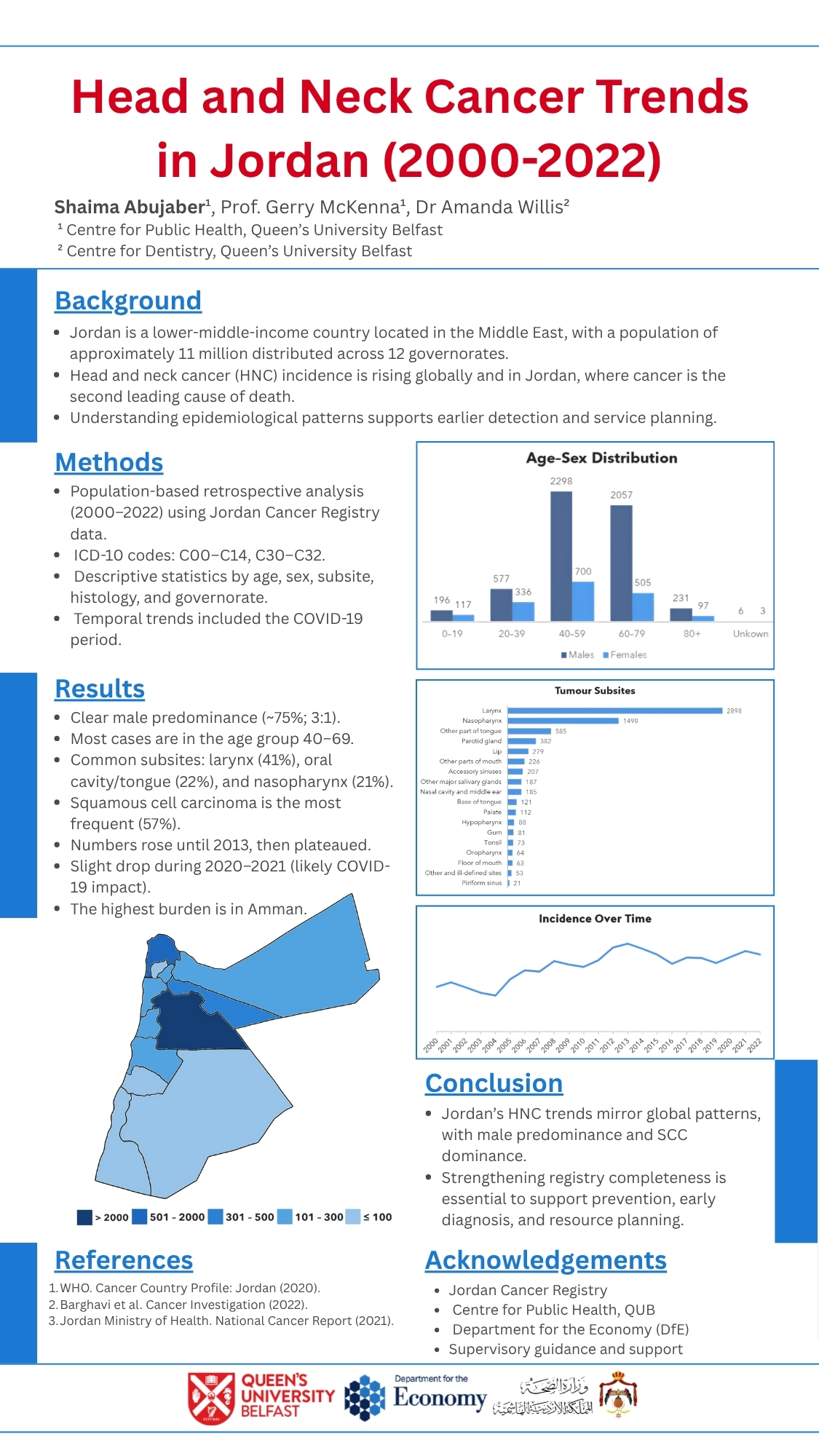
This study provides a preliminary overview of trends in head and neck cancer (HNC) in Jordan by analysing demographic, anatomical, and histological patterns over the past two decades using national registry data.
Design:
Retrospective, population-based observational study.
Setting:
The Hashemite Kingdom of Jordan is a Middle Eastern country with a population of approximately 11 million. Data were obtained from the Jordan Cancer Registry (JCR), a national registry that captures all cancer diagnoses.
Participants:
Newly diagnosed HNC patients in Jordan, recorded in the Jordan Cancer Registry from 2000 to 2022.
Main Outcome Measures:
Descriptive analyses of age, sex, tumour site, and histology were conducted. Trends in annual case numbers and mortality rates were also examined, where data were available.
Results:
Most patients were male (5,365; 75%), with a male-to-female ratio of approximately 3:1. The age at diagnosis ranged mainly from 40 to 69 years. The most common subsites were laryngeal (2,898; 41%), oral cavity/tongue (1,520; 22%), and nasopharyngeal cancers (1,498; 21%). Squamous cell carcinoma accounted for about 57% of tumours. Death data were available for approximately 85% of Jordanian patients, with most deaths occurring between 55 and 79 years (median around 65–70 years). Annual case numbers increased gradually in the early 2000s, peaking around 2013, stabilising after 2015, with minor disruptions related to COVID-19 (2020–2021).
Conclusion:
This preliminary analysis provides the first comprehensive overview of HNC trends in Jordan, highlighting demographic, anatomical, and histological patterns over twenty years. Although some variables, such as histological grade (~41%), tumour stage (~40%), and death status (~15% of Jordanians), were not fully recorded, the dataset remains highly informative. Limited follow-up for non-Jordanians and missing information on lifestyle factors, TNM staging, and treatment highlight opportunities for improved data collection in future registry updates. These findings can inform prevention, early detection, and future research efforts within the Jordanian population.
Note:
This abstract presents a preliminary analysis of registry data; a manuscript has not yet been drafted.