Hypoglossal Nerve Palsy as the Primary Clinical Presentation of Carotid Artery Dissection
unknown
Caitlin Wren
Caitlin Wren, Imola Virginas
History:
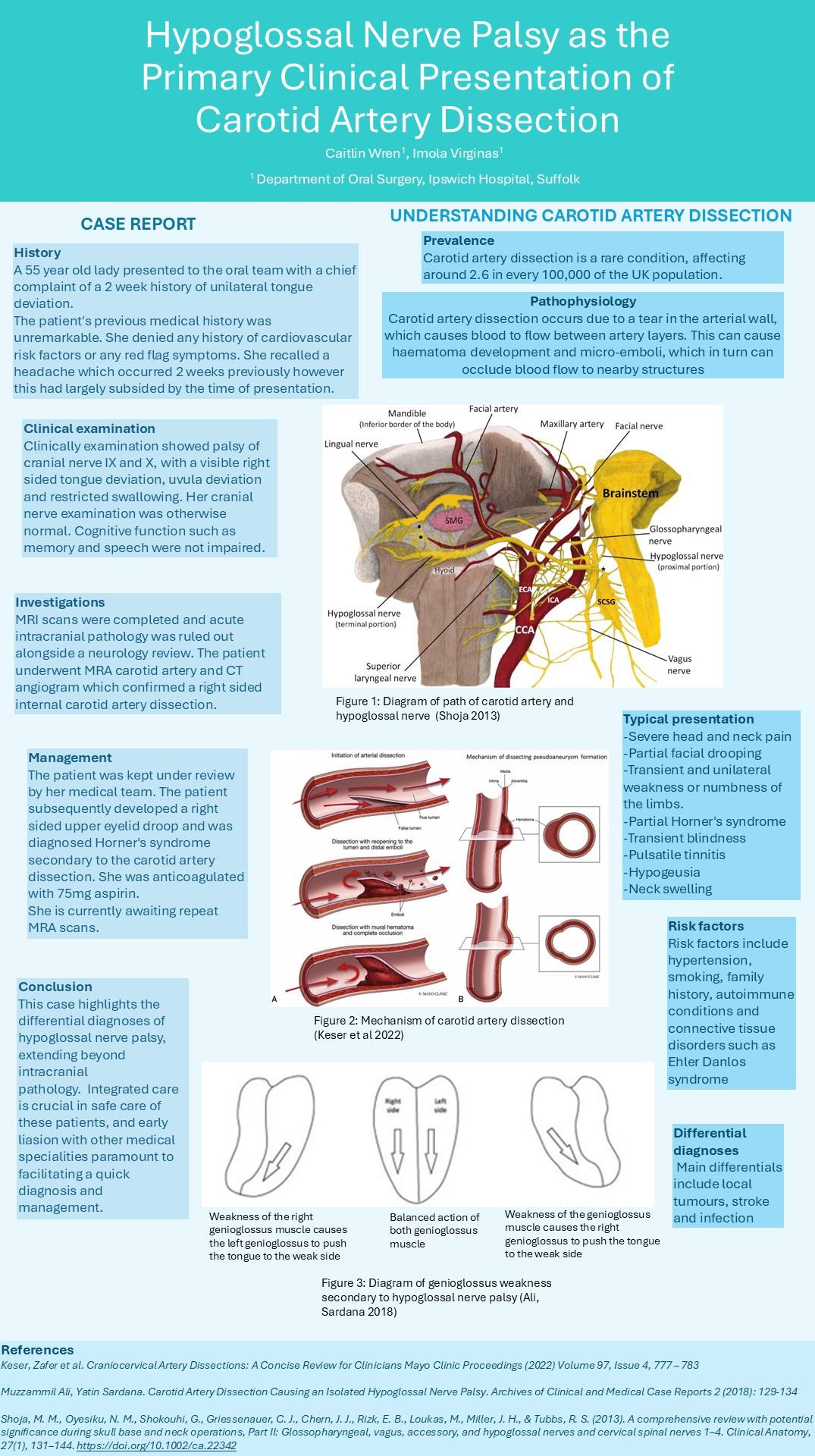
A 55 year old lady presented to the oral team with a chief complaint of a 2 week history of unilateral tongue deviation.
The patient’s previous medical history was unremarkable. She denied any history of cardiovascular risk factors or any red flag symptoms. She recalled a headache which occurred 2 weeks previously however this had largely subsided by the time of presentation.
Clinical examination:
Clinically examination showed palsy of cranial nerve VIll and VI with a visible right sided tongue deviation, uvula deviation and restricted swallowing. Her cranial nerve examination was otherwise normal. Cognitive function such as memory and speech were not impaired.
Investigation:
MRI scans were completed and acute intracranial pathology was ruled out alongside a neurology review. The patient underwent MRA carotid artery and CT angiogram which confirmed a right sided internal carotid artery dissection.
Management:
The patient was kept under review by her medical team. The patient subsequently developed a right sided upper eyelid droop and was diagnosed Horner’s syndrome secondary to the carotid artery dissection. She was anticoagulated with 75mg aspirin.
She is currently awaiting repeat MRA scans.
Conclusion:
This case highlights the differential diagnoses of hypoglossal nerve palsy, extending beyond intracranial pathology. These can include local tumours, haematological malignancies, stroke and infection. Integrated care is crucial in safe care of these patients, and early liason with other medical specialities paramount to facilitating a quick diagnosis and management.