Immunobullous Crossroads: Navigating Serological Overlap Between Pemphigus and Pemphigoid Without Paraneoplastic Autoimmune Multiorgan Syndrome
CR13
Sohum Pandya
Sohum Pandya, Alexandra Perks, Andrea Richards, Georgina Fremlin
We present a rare case of immunobullous disease with serological features of both pemphigus vulgaris (PV) and mucous membrane pemphigoid (MMP), in the absence of paraneoplastic autoimmune multiorgan syndrome (PAMS).
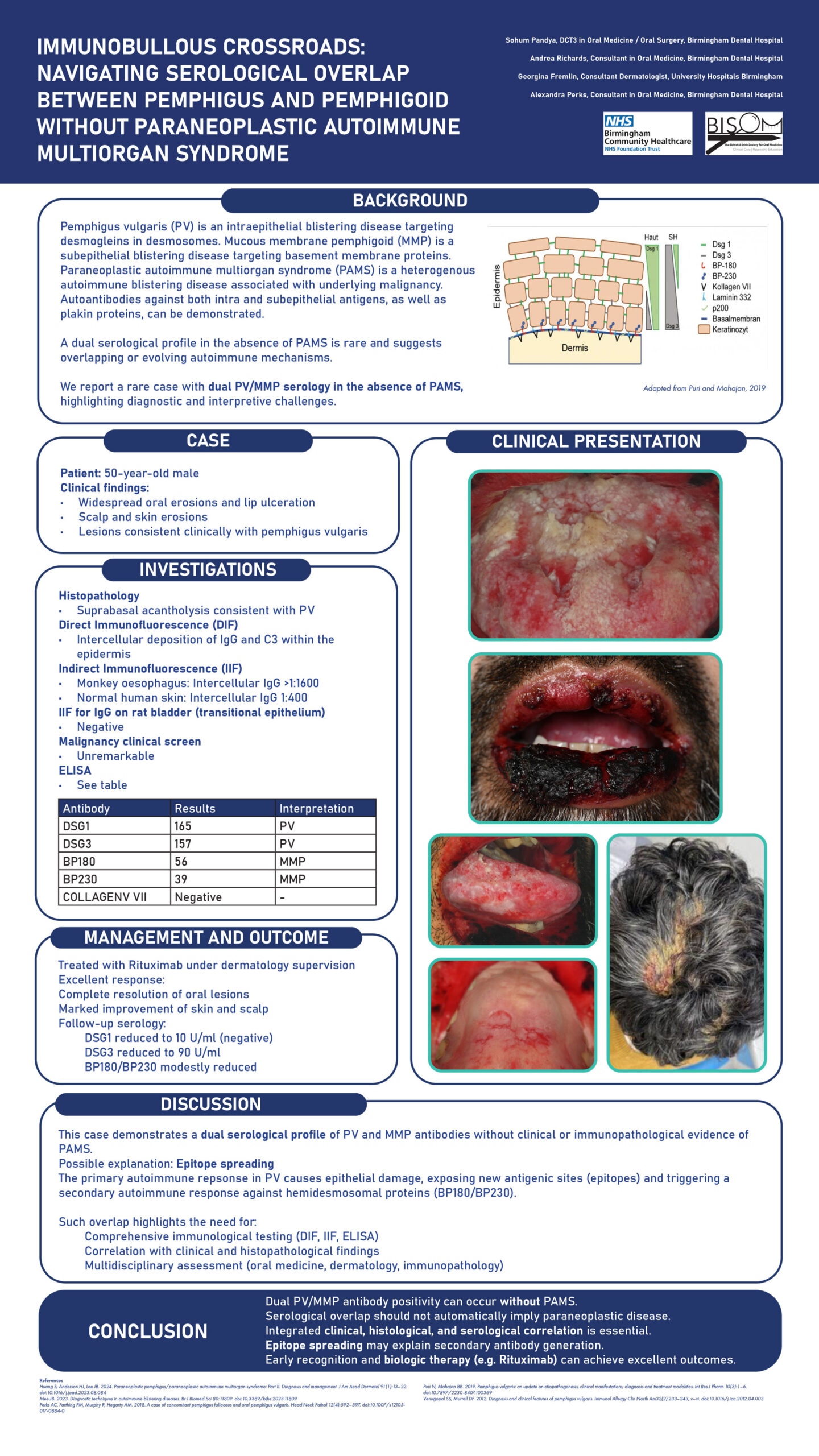
A 50-year-old male presented with significant and widespread oral erosions, lip ulceration, and erosions of the scalp and skin. Clinically, the distribution and morphology were consistent with PV. Histological features from a cutaneous biopsy confirmed PV, and direct immunofluorescence (DIF) demonstrated intercellular deposition of IgG and C3 within the epidermis.
Indirect immunofluorescence (IIF) revealed high-titre intercellular IgG antibodies on monkey oesophagus (>1/1,600) and normal human skin (1/400). ELISA detected anti-DSG1 antibodies (165 U/ml) and anti-DSG3 antibodies (157 U/ml), consistent with PV, but also revealed anti-BP180 (56 U/ml) and anti-BP230 antibodies (39 U/ml), more typical of MMP. IIF for IgG on rat bladder (transitional epithelium) and ELISA for anti-collagen VII were both negative.
Given the dual serological profile, PAMS was considered. Expert review from the St John’s Institute of Dermatology concluded this was unlikely, as IIF on transitional epithelium was negative and DIF showed pemphigus-pattern only. Additionally, the patient was clinically well, and a full malignancy screen was unremarkable, so CT imaging was not indicated.
The patient was successfully treated with Rituximab under dermatology care. Oral lesions completely resolved, and skin and scalp improved significantly. Follow-up serology showed anti-DSG1 antibodies had become negative (10 U/ml), anti-DSG3 reduced to 90 U/ml, with modest reductions in anti-BP180 and BP230.
This dual antibody profile without PAMS may be explained by a phenomenon called epitope spreading, whereby the primary autoimmune response leads to tissue damage revealing new antigenic sites (epitopes), triggering a secondary autoimmune response.
This case highlights the diagnostic complexity of immunobullous diseases and the need for integrated clinical, histological, immunological, and multidisciplinary assessment.