Oral and Systemic Manifestations of Hereditary Haemorrhagic Telangiectasia
CR 18
Lewis Olsson
Lewis Olsson, Clare Marney
Background:
Hereditary haemorrhagic telangiectasia (HHT) is a rare autosomal dominant vascular disorder characterized by mucocutaneous telangiectasias and visceral arteriovenous malformations (AVMs). The oral cavity is commonly involved. HHT prevalence is estimated at 1 in 5,000 individuals. Early recognition is important due to the risk of life-threatening haemorrhage and complications such as cerebral abscess.
Case:
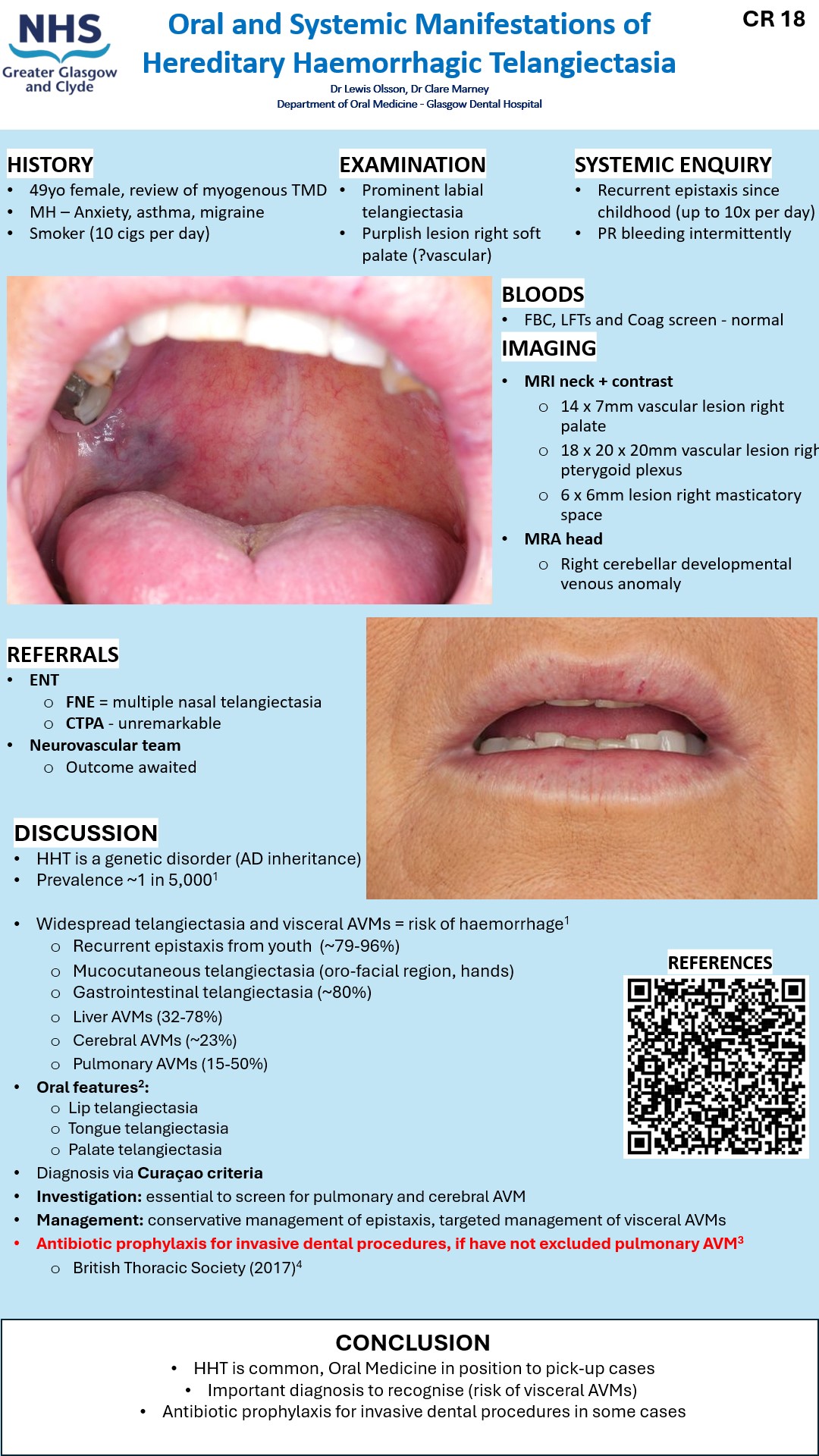
A 49-year-old female was referred to Oral Medicine with TMD. Background included asthma, anxiety, depression, and tobacco use. Clinical examination revealed incidental upper and lower lip telangiectatic lesions and a vascular mucosal lesion right soft palate. Further questioning revealed a significant history of epistaxis. MRA head and neck demonstrated a 14 × 7 mm lesion AVM right palate as well as lesions right pterygoid plexus and right masticatory space. Patient was referred onward to ENT, nasal endoscopy confirmed multiple nasal telangiectasias. Further imaging ruled out pulmonary and cerebral AVMs. A diagnosis of HHT was established, and management included nasal emollients and referral to neurovascular surgical team.
Discussion:
HHT commonly presents with recurrent epistaxis (79–96%), mucocutaneous telangiectasias, and AVMs affecting the gastrointestinal tract, liver, lungs, and brain. Diagnosis is established via the Curacao criteria. Oral manifestations include telangiectasias of the lips, tongue, and palate and may result in troublesome bleeding requiring surgical intervention. Screening for pulmonary and cerebral AVMs is a priority. Guidance recommends antibiotic prophylaxis prior to invasive dental procedures in patients with pulmonary AVMs due to a 500-fold increased risk of cerebral abscess.
Conclusion:
Clinicians should maintain a high index of suspicion for HHT in patients with unexplained epistaxis and oral telangiectasias. Multidisciplinary management and imaging are vital to exclude visceral AVMs and prevent complications. Oral Medicine play a key role in identifying oral features and coordinating appropriate imaging and onward referrals.