Blistering of the Palate with Unusual Skin Lesions: A Case Report
A10
Junaid Rashid (1)
Timothy Bates (2), Shireen Velangi (3), Rachel Brown (2), Andrea Richards (1), Jon Higham (1), Ana Poveda-Gallego (1), Alexandra Perks (1)
Introduction
Fixed drug eruption (FDE) is a cutaneous adverse reaction characterised by recurrent lesions at the same site upon exposure to the causative drug. Skin lesions present as well-demarcated, erythematous plaques or macules, occasionally accompanied by bullae and erosion. Oral involvement is rare. Causative drugs include nonsteroidal anti-inflammatory drugs (NSAIDs), paracetamol, and antifungals. We present a unique case of FDE affecting oral mucosa and skin, triggered by etoricoxib.
Case Report
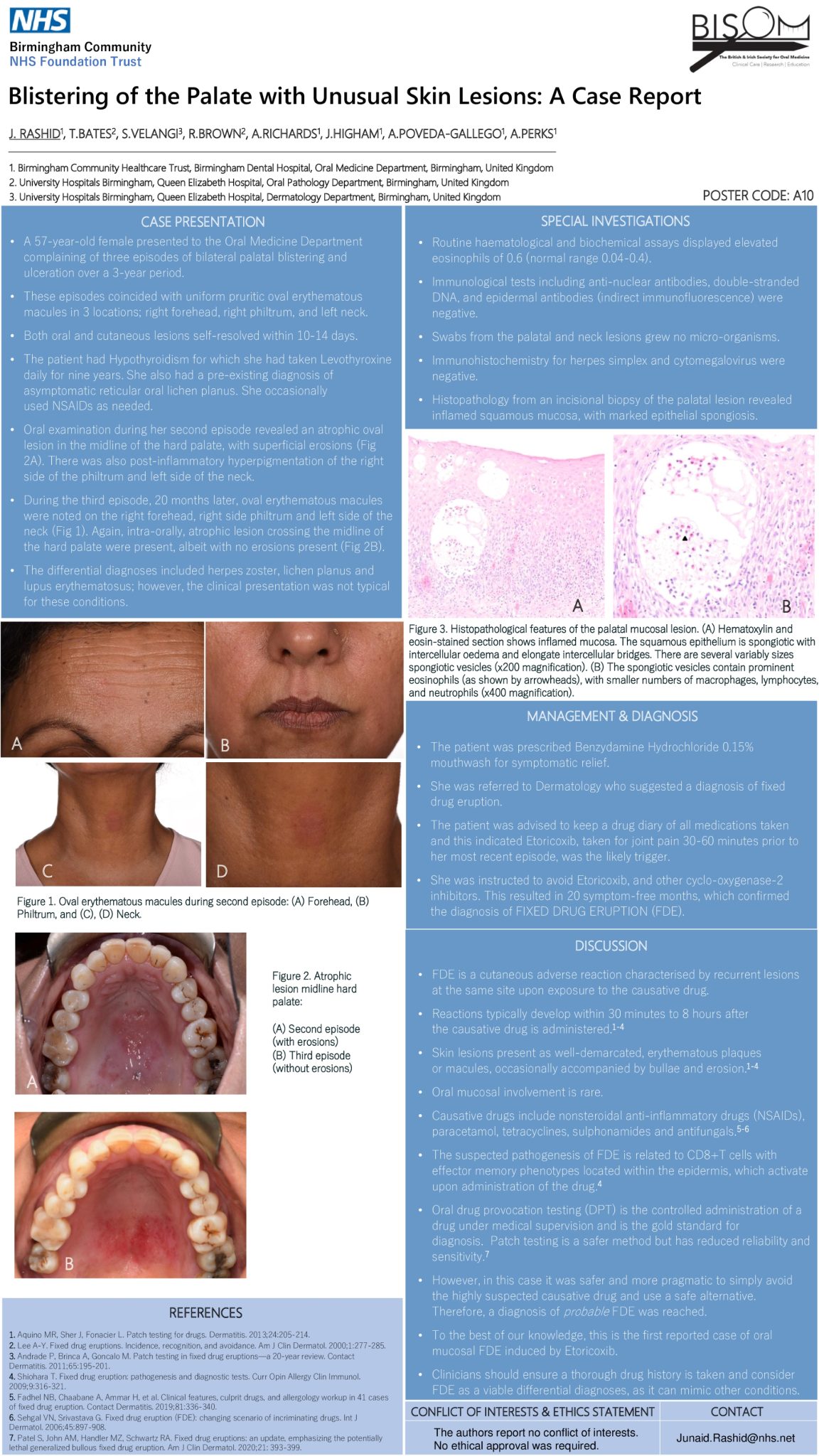
A 57-year-old female presented to the Oral Medicine Department complaining of three episodes of palatal blistering and ulceration. These episodes coincided with uniform pruritic oval erythematous macules on the right forehead, right philtrum, and left neck, which self-resolved within 10-14 days. She had a preexisting diagnosis of reticular oral lichen planus and a nine-year history of daily levothyroxine use for hypothyroidism. She occasionally used NSAIDs as needed and was a non-smoker.
Examination revealed an atrophic oval lesion in the midline of the hard palate, with superficial erosions. Differential diagnoses included herpes zoster, lichen planus, and lupus erythematosus. For symptomatic relief, the patient was prescribed Benzydamine Hydrochloride 0.15% mouthwash. Blood tests revealed elevated eosinophils, and histopathology from the palatal biopsy revealed eosinophilic spongiosis. Immunohistochemistry for herpes simplex virus and cytomegalovirus returned negative.
She was referred to Dermatology who suggested a diagnosis of FDE. A retrospective drug diary indicated that etoricoxib, taken 30-60 minutes before her latest episode was the likely trigger. A diagnosis of probable FDE induced by etoricoxib was established. She was advised to avoid etoricoxib and other cyclooxygenase-2 inhibitors, resulting in 20 symptom-free months, after which she was discharged.
Conclusion
Intra-oral mucosal manifestation of FDEs and eosinophilic spongiosis are rarely encountered. Clinicians should consider FDEs in their list of differential diagnoses as they can mimic other conditions. Therefore, it’s imperative clinicians obtain a comprehensive drug history for all patients.