Calcium Pyrophosphate Deposition Disease (CPPD), or Pseudogout, of the Temporomandibular joint: an unusual condition
A13
Manveer Singh Chhina
Manveer Singh Chhina, Clare Marney & Orlagh McPolin
Introduction
Calcium pyrophosphate deposition disease (CPPD) or pseudogout, is a form of arthritis that causes severe inflammation of the joints resulting in acute pain, swelling and limitation of function [1]. Although the aetiology is not fully understood, the key feature is formation of pyrophosphate crystals in cartilage or synovial fluid, triggering a severe inflammatory response [2].
Although the majority of temporomandibular dysfunction (TMD) presentations are due to myofascial pain and meniscal derangement, the TMJ can less commonly be affected by inflammatory arthropathies such as psoriatic arthritis, rheumatoid arthritis and ankylosing spondylitis [3]. There are few reported of cases in the literature of pseudogout of TMJ.
Methodology
An 84-year-old female presented to the Oral Medicine department with a 6-day history of sudden onset pain in the right face, localising to TMJ and parotid gland. She denied any other joint symptoms, fever, weight loss or sweats. The patient had no relief from Paracetamol but some benefit from Ibuprofen. Examination revealed trismus, tenderness, erythema and oedema overlying the right TMJ and parotid.
Investigations
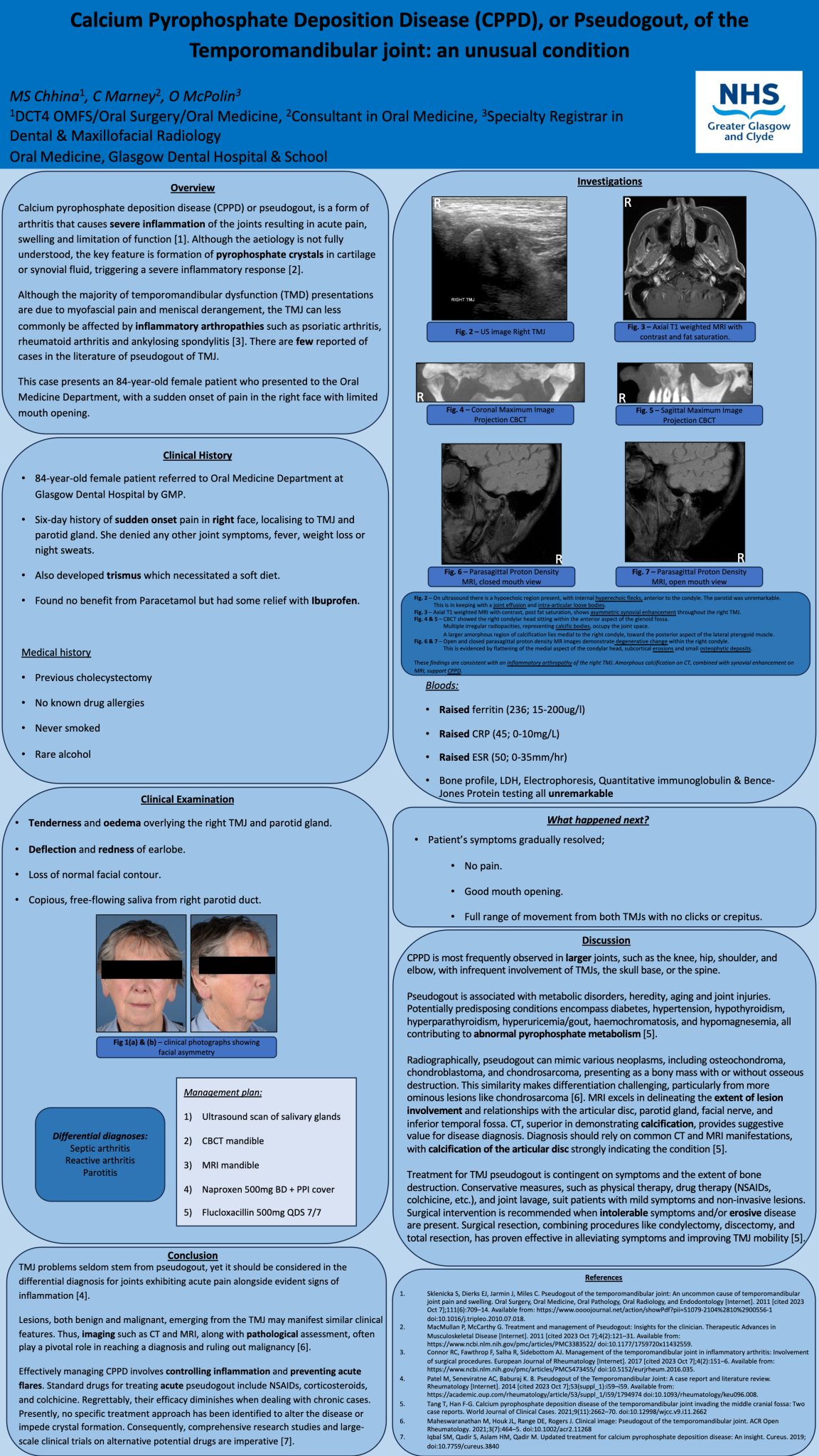
Blood tests revealed raised ferritin (236; 15-200ug/l), CRP (45; 0-10mg/L) and ESR (50; 0-35mm/hr). The right parotid gland was unremarkable on ultrasound scan, but there was evidence of joint effusion and intra-articular loose bodies in the right TMJ.
CBCT and MRI of TMJs were taken which showed evidence of inflammatory arthropathy, with loose calcific bodies and irregular radiopacities within the joint space and muscle, but no gross bony changes. These features suggested pseudogout, but differential diagnoses included previous haematoma or neoplasia.
Conclusion
TMJ issues are rarely a result of pseudogout but it should be included in the differential diagnosis for acutely painful joints with definite signs of inflammation [4]. It can be treated with non-steroidal anti-inflammatories or conservative arthroplasty, or with surgical resection and reconstruction in more severe cases [5].