Facial numbness, not to be taken lightly: A case series
BR69WD
AAYA SHAMEKH
Molly Harte1 , Sandeep Joshi1 , Rui Albuquerque1 , Richard Cook1,2
Title: Facial numbness, not to be taken lightly: A case series
Authors: Aaya Shamekh, Molly Harte, Sandeep Joshi, Rui Albuquerque, Richard Cook
Background
In Oral Medicine, orofacial numbness and tingling frequently presents as a feature of trigeminal neuropathy or persistent idiopathic facial pain (PIFP)1. However, orofacial numbness can be a manifestation of a much broader range of pathology, from oral cancer to dental infection2. We present three cases of CNV mandibular division numbness seen in Oral Medicine at Guy’s Hospital, with very different underlying pathologies.
Cases
Case 1: A 28-year-old male presented with a 6-month history of intermittent tingling of the left tongue. MRI and CBCT showed an inferiorly impacted LL8 with a dentigerous cyst, thinning the lingual cortical plate and displacing the ID canal inferiorly.
Case 2: A 45-year-old female presented with a 7-month history of numbness/tingling in the lower right quadrant, lower right lip and chin. The LR8 had mesial caries but no frank apical pathology was seen on OPG. MRI demonstrated marrow signal heterogeneity in the right distal mandible. Subsequent CBCT showed spreading infection arising from the carious LR8, impacting the roof of the right ID canal with communication.
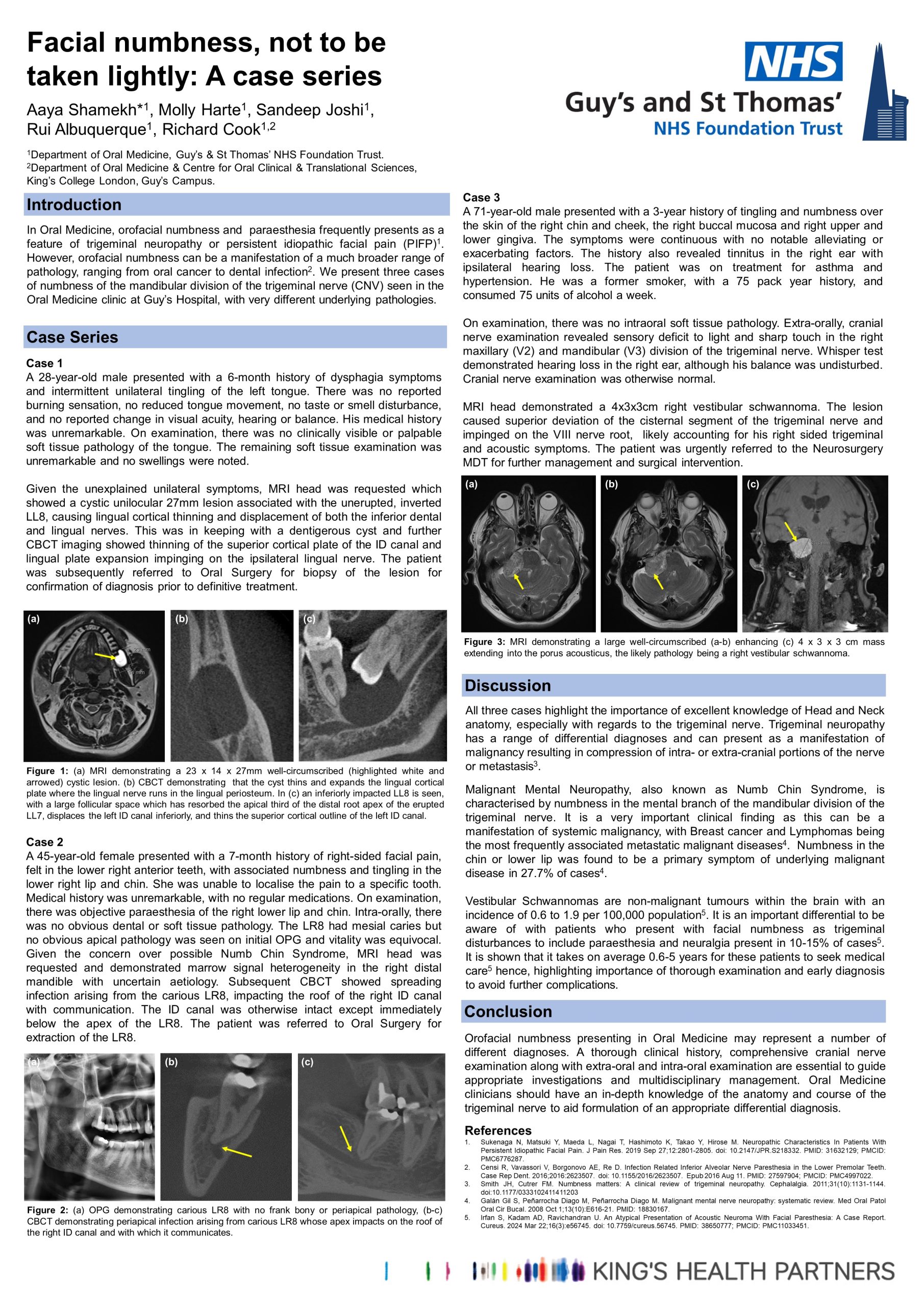
Case 3: A 71-year-old male presented with a 3-year history of tingling/numbness over the right facial skin in the CNV12 divisions, the right buccal mucosa and right upper and lower gingiva. Questioning revealed a history of tinnitus in the right ear with ipsilateral hearing loss. MRI demonstrated a 4x3x3cm right vestibular schwannoma, causing superior deviation of the cisternal segment of the trigeminal nerve, accounting for his symptoms.
Conclusion
Orofacial numbness presenting in Oral Medicine may be labelled as PIFP. The differential diagnoses for patients presenting with these symptoms are broad, and whilst PIFP is a possible cause, other aetiologies including odontogenic pathology and neoplasms should be considered. A thorough clinical history, comprehensive cranial nerve and intra-oral examination, and sometimes multi-modal imaging investigations are essential for accurate diagnosis and timely intervention.
References
1. Sukenaga N, Matsuki Y, Maeda L, Nagai T, Hashimoto K, Takao Y, Hirose M. Neuropathic Characteristics In Patients With Persistent Idiopathic Facial Pain. J Pain Res. 2019 Sep 27;12:2801-2805. doi: 10.2147/JPR.S218332. PMID: 31632129; PMCID: PMC6776287.
2. Censi R, Vavassori V, Borgonovo AE, Re D. Infection Related Inferior Alveolar Nerve Paresthesia in the Lower Premolar Teeth. Case Rep Dent. 2016;2016:2623507. doi: 10.1155/2016/2623507. Epub 2016 Aug 11. PMID: 27597904; PMCID: PMC4997022.