The development of severe dysplasia in a patient with successfully-treated paraneoplastic pemphigus: a case report
7493
Sarah Young
Sarah Young, Claire M Healy, Esther O'Regan, Sheila Galvin
Introduction: Paraneoplastic pemphigus (PNP) is a rare, autoimmune-mediated, blistering, mucocutaneous disease which is almost always associated with a confirmed neoplasm. We present a case of a 49-year old female with paraneoplastic pemphigus secondary to Castleman’s Disease.
Case summary:
The patient was referred with a 4 month history of severe and progressive oral ulceration, unresponsive to topical steroids with associated itchy skin rash and genital irritation. She had no prior medical history, took no medications, never smoked and consumed minimal alcohol. Examination showed erythematous papules with occasional vesicles on the arms, fingertips and neck. Intra-orally, there was extensive ulceration of the tongue, buccal and labial mucosae, palate and gingiva. The clinical findings were suggestive of an immunobullous disorder and she was commenced on high-dose oral prednisolone. Histopathology was suggestive of erythema multiforme, however direct immunofluorescence showed linear IgG and IgM and granular C3 along the mucosal-submucosal junction and IgG and C3 staining of junctional intercellular spaces suggestive of PNP.
Subsequent CT-TAP revealed a large retroperitoneal mass, with biopsy confirming Castleman’s Disease. Surgical resection of the mass was followed by low dose radiotherapy. Her oral ulceration resolved with disease control, resulting in mucosal atrophy and scarring.
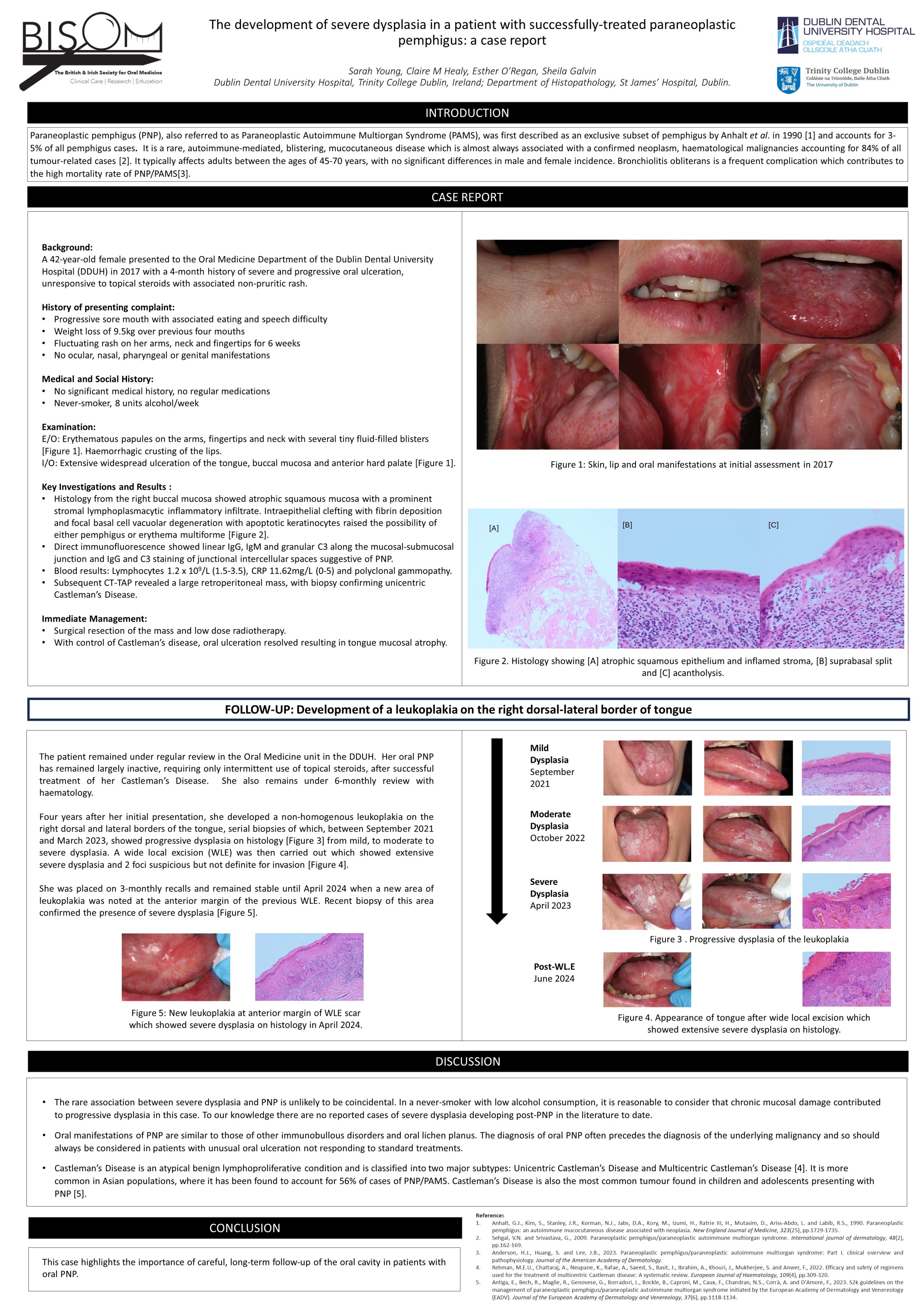
Four years after initial presentation she developed a leukoplakia on the right dorso-lateral tongue, serial biopsy of which showed progression from mild to moderate to severe dysplasia. Subsequent wide local excision showed extensive severe dysplasia. She remains under close monitoring in the oral mucosal dysplasia clinic.
Conclusion: The rare association between severe dysplasia and PNP is unlikely to be coincidental. In the absence of risk factors such as smoking and alcohol, it is reasonable to consider that chronic mucosal damage contributed to progressive dysplasia in this case. This highlights the importance of careful, long-term follow-up of the oral cavity in patients with oral PNP.