Uraemic Stomatitis: a Rare Complication of Chronic Kidney Disease – a Case Report
CR9
Kamila Marcinczak
Sheila Galvin, Claire Healy
Background:
Uraemic stomatitis is a rare complication of chronic kidney disease, typically associated with end-stage renal disease (ESRD). It results from the accumulation of uraemic toxins, which are excreted in saliva and hydrolyzed by oral bacterial ureases to produce ammonia. Ammonia irritates the oral mucosa, leading to inflammation, ulceration and pseudomembranous plaques.
Case Presentation:
A 24-year-old student with ESRD secondary to polycystic kidney disease was referred to the Oral Medicine Department by her nephrologist with a 6 month history of progressive, white plaques on the oral mucosa. These were unresponsive to various topical and systemic anti-fungal treatments. She complained of an unpleasant sensation and halitosis but was otherwise asymptomatic. A poor AV fistula and the patient’s wish to complete her studies had delayed haemodialysis, and she was awaiting renal transplantation. She had secondary hyperparathyroidism and anaemia. She was a non-smoker and did not drink alcohol.
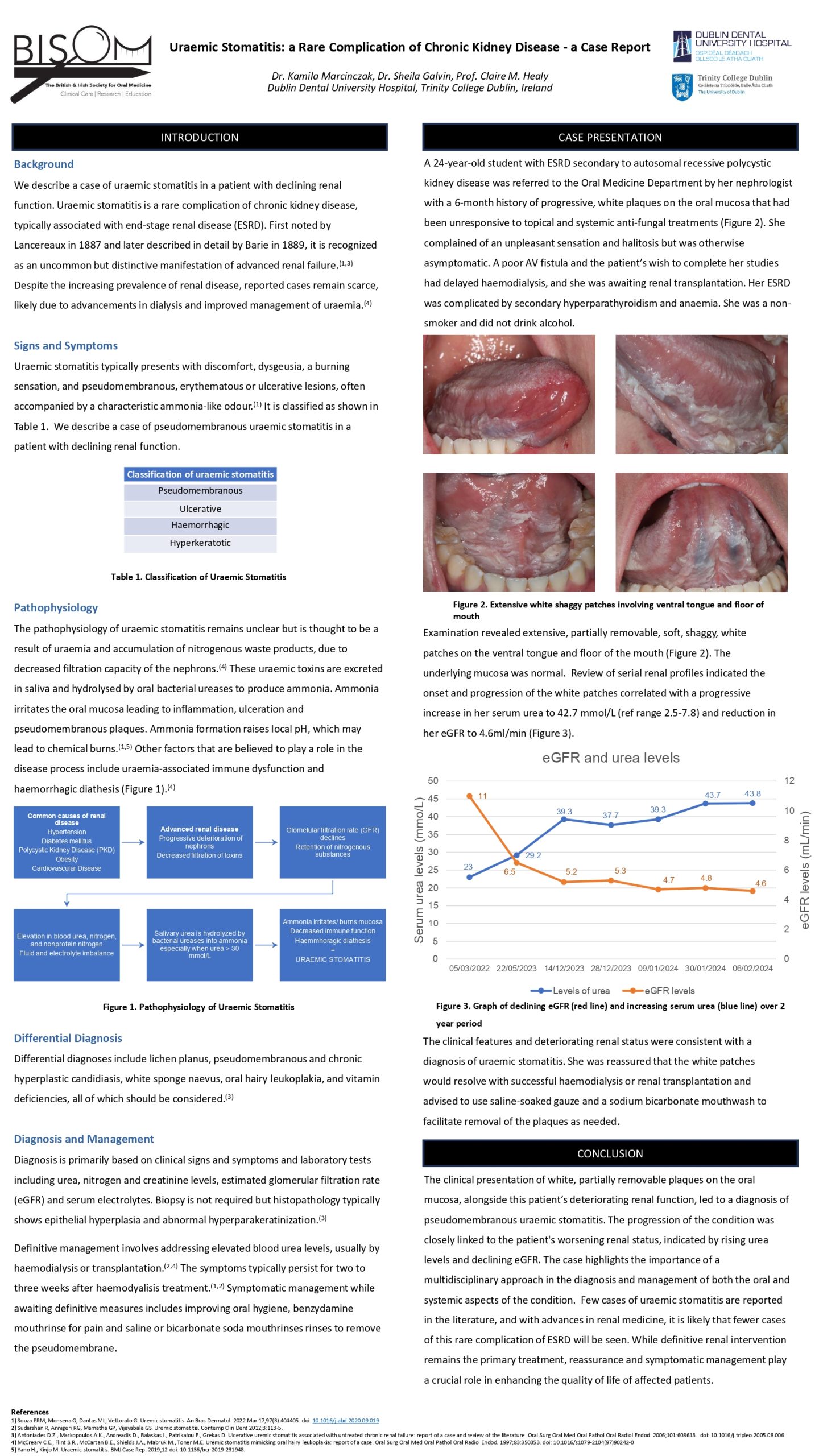
Examination revealed extensive, partially removable, soft, shaggy, white patches on the lateral and ventral tongue and floor of the mouth. The underlying mucosa was normal. Review of serial renal profiles indicated the onset and progression of the white patches correlated with a progressive increase in her serum urea up to 42.7 mmol/L (ref range 2.5-7.8) and reduction in her eGFR to 4.6ml/min. The clinical features and deteriorating renal status indicated a diagnosis of uraemic stomatitis. She was reassured that the white patches would resolve with successful haemodialysis or renal transplantation and advised to use saline-soaked gauze and a sodium bicarbonate mouthwash to facilitate removal of the plaques.
Conclusion:
Few cases of uraemic stomatitis are reported in the literature, and with advances in renal medicine, it is likely that fewer cases of this rare complication of ESRD will be seen.
Reassurance and symptomatic management enhance quality of life in these patients while awaiting definitive renal intervention.